Mini Innovation Challenge #1
Provide a clear, concise problem statement describing a challenge you or your patients face in the acute care/emergency setting.
Winner
James Orlando Jordano
M4, Vanderbilt University School of Medicine
With emergency department (ED) boarding a nationwide problem, quick yet safe disposition and discharge has been more important than ever. However, there remains one population that continually has slower disposition, higher financial burden on hospitals, and still worse health outcomes: patients experiencing homelessness. Studies have shown that patients experiencing homelessness use the ED more than the average population, with one study recording 39 patients returning to the ED for 347 visits during a 40-month period.(1) To safely discharge these patients, social workers are forced to quickly mobilize resources. They recognize the longer it takes to identify a safe discharge plan, the longer the patient will be in the ED—leading to worse patient health outcomes, higher cost to the hospital, and a decreased total number of patients seen by an ED provider. The result is instinctive referrals to the same local resources, regardless of age, gender, disability, and access from encampment site. This ultimately leads to poor follow-up and re-presentation to the ED, thus restarting the cycle. While already taxing, this issue will only continue to grow; from 2018 to 2019 the number of people experiencing homelessness grew by nearly 15,000,(2) further challenging the healthcare system to find a better solution.
-
One solution is a “social needs room.” Once a patient is medically cleared, they can be discharged to this intermediate location within the hospital. In this room, patients can wait comfortably for a social worker—assigned to work with this suite of patients directly—to carefully tailor local resources based on relevant patient statuses and their accessibility to the patient’s home encampment. From a provider perspective, this would allow another patient to be seen in the ED. From a hospital perspective, the cost of running a social needs room would be far lower than the cost of holding a patient in the ED while awaiting disposition, as it would only need a social worker instead of a social worker, doctors, and nurses. Finally and most importantly, from a patient perspective, these patients will still have a space for shelter while awaiting disposition. There, they will receive personalized resources and more realistic follow-up plans with local free clinics and/or street medicine services. With multiple studies in support, improved hospital follow-up for patients experiencing homelessness will ultimately decrease the rate of re-presentation to the ED and improve health outcomes.(3,4)
Finalist
SimileOluwa Onabanjo
Medical Officer, Lagos State University Teaching Hopital
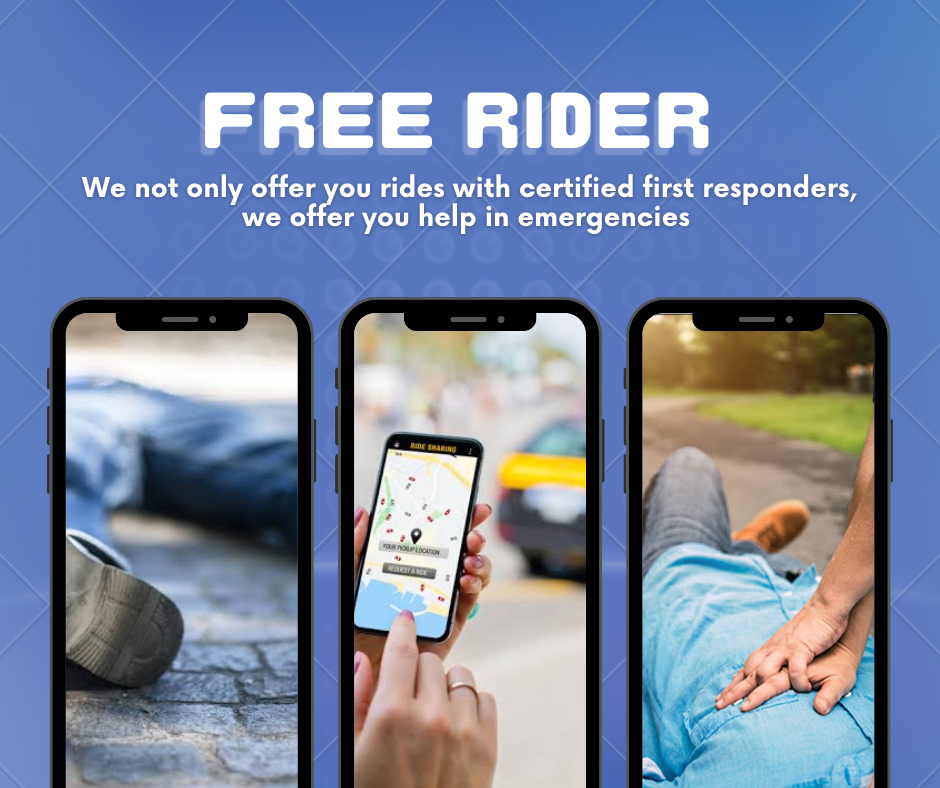
Many factors have been associated with poor outcomes following out-of-hospital sudden cardiac arrest (OHSCA), however, one of the most important factors identified is the time elapsed prior to effective resuscitation. This includes delayed administration of effective bystander cardiopulmonary resuscitation (CPR) and delayed defibrillation.
Studies performed in developing studies, particularly in those with underdeveloped emergency care systems show a very poor uptake of bystander CPR and unavailability of Automated External Defibrillators. A limitation noted in one of these studies included the fear of causing further harm which was attributed to a poor level of knowledge and practice of CPR. This has significantly contributed to the poor survival rate seen in out-of-hospital cardiac arrests.
In many developing countries, knowledge of lifesaving skills remains the exclusive preserve of healthcare workers. To reduce mortalities of OHSCAs in developing countries, it is important to effectively equip lay first responders with adequate knowledge of CPR including the use of AEDs as this will significantly shorten the time gap between the occurrence of OHSCA and administration of effective CPR.
-
Transportation, including public and private means is a vital part of our daily lives. This makes transport workers a very vital target population for lay first responder training. Transport workers, especially those employed by commercial companies with ride-hailing applications can be trained as lay first responders. An SOS option can be included on ride-hailing applications associated with these companies to alert drivers of nearby emergencies with specific locations. Drivers can be rated based on their promptness and professionalism to add as an incentive. Also, a digital log should also be added to these applications t keep track of cases and their outcomes. Bi-annual refresher trainings should also be organized for these workers. This is a win-win situation as it improves timeliness of effective resuscitation during emergencies and improves the visibility, relevance and use of these apps, thereby also increasing income generation.
Finalist
Megan Amber Lin
MS1, University of Illinois, Urbana Champaign
Patients presenting to the emergency department (ED) likely have past medical histories with networks of various providers dedicated to their health conditions. Quickly accessing this background information and these providers’ perspectives is essential for the ED physician’s understanding of the patient’s chief complaint and formation of their entire story. Due to the immediate demand of the patient’s situation, efficiency of clinician-clinician communication becomes ever more critical. However, there currently is a lack of technology linking real-time communication and discussion between the providers falling under each individual patient. Instead of having a direct way to reach the patient’s providers in a collaborative space and gather all input in a centralized fashion, the ED clinicians must make individual consultations to eventually piece together the underlying story of the patient.
A software-enabled chatroom amongst these providers that can be accessed online through login of the electronic medical record (EMR) is needed. This virtual, real-time conferencing would enable clinicians to more quickly gain a holistic understanding of their patients in urgent situations and empower them to make the most informed decision.